
Antidote, Nerve Agent (CANA) autoinjector for the immediate field treatment. However, benzodiazepines are less effective at terminating seizures when given 30 min or later after OP exposure or seizure onset, likely because of internalization or downregulation of synaptic, but not extrasynaptic, GABAA receptors, which can lead to diminished potency and seizure recurrence. The drug midazolam has been recommended to replace diazepam as the immediate. SIGNIFICANCE: In experimental models, midazolam is effective when given at the onset of seizures caused by nerve agents. Clinical studies such as the recent Rapid Anticonvulsant Medication Prior to Arrival Trial (RAMPART) trial have confirmed the anticonvulsant efficacy of midazolam in SE in prehospital settings. Due to its favorable pharmacokinetic features, midazolam is being considered as a replacement anticonvulsant for diazepam in the antidote kit for nerve agents.


Midazolam is administered intravenously or intramuscularly to control acute seizures and SE. Other useful information pertaining to the use of each drug is presented, such as: central or peripheral line recommendations. It potentiates GABAergic inhibition and thereby controls hyperexcitability and seizures. Midazolam is a positive allosteric modulator of synaptic γ-aminobutyric acid (GABA)A receptors in the brain.
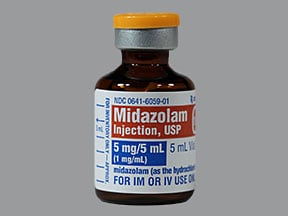
RESULTS: Midazolam is considered the new drug of choice for persistent acute seizures and SE, including those caused by neurotoxic OPs and nerve agents. Midazolam is a benzodiazepine hypnotic with a rapid onset and short duration of action. METHODS: Benzodiazepines are widely used to treat acute seizures and status epilepticus (SE), a neurologic emergency of persistent seizures that can lead to severe neuronal damage or death. OBJECTIVE: This review summarizes the therapeutic potential of midazolam as an anticonvulsant antidote for organophosphate (OP) intoxication.


 0 kommentar(er)
0 kommentar(er)
